En atención a la creciente preocupación sobre la confianza en...
Leer más
This Is Your Brain on COVID-19

Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr F. Perry Wilson of the Yale School of Medicine.
SARS-CoV-2 is a strange virus, and not only because it is so novel. The variability in clinical presentation and outcome is still perplexing; the emergence of variants like Omicron, with few links to established lineages, is weird; and then there is the anosmia.

In retrospect, it may have been our first clue that the virus that causes COVID-19 was an odd bird — the high prevalence of the loss of the sense of smell. It’s an unusual symptom, and even in early studies stood out as a powerful predictor that the upper respiratory syndrome a patient was presenting with was caused by COVID and not flu or another cold virus.
At first, there was speculation that the loss of smell was simply a symptom of stuffed nasal passages, but this theory quickly evaporated, as many patients reported prolonged loss of smell even long after the infection had subsided. SARS-CoV-2, it seemed, might be able to affect the brain itself.
Anyone who has taken care of COVID patients in the hospital will confirm that the nervous system is not spared in many cases. COVID neuropathy, and COVID delirium, are not uncommon. But exactly how COVID affects nervous tissues has been really hard to untangle.
But this week, in JAMA Network Open, we have a decent effort to start to pull some of those threads, thanks to data from spinal taps.
Researchers led by Arvid Edén, from Sweden, went right to the source by examining the cerebrospinal fluid of patients hospitalized with COVID.
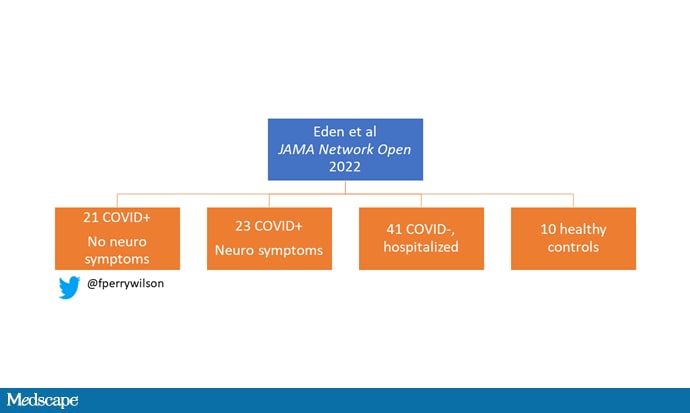
This is a study of multiple cohorts, broken down here. We have 21 patients with COVID and nervous system pathology — primarily encephalopathy; 23 patients with COVID and no nervous system problems; 41 hospitalized patients without COVID; and 10 healthy controls.
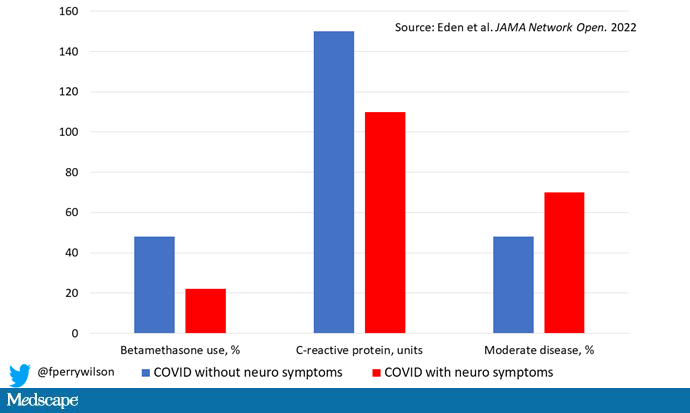
What struck me right away was the fact that, by and large, the COVID patients with nervous system findings seemed less sick at baseline than those without. They were less likely to be receiving betamethasone, a steroid, for instance. They had a lower C-reactive protein, a marker of inflammation, and were more likely to have moderate disease compared with severe disease, according to the WHO classification.
This raised my eyebrows a bit. After all, if someone is severely ill with COVID, potentially intubated and sedated, how would you know whether they had nervous system pathology at all? The authors don’t report on the use of sedation, unfortunately. But bear it in mind as we examine the characteristics in the spinal fluid of these patients.
Okay. The big finding: None of these patients — zero — had COVID RNA in their CSF. Put another way, there is really no evidence, in this study, of direct infection of brain cells by SARS-CoV-2.
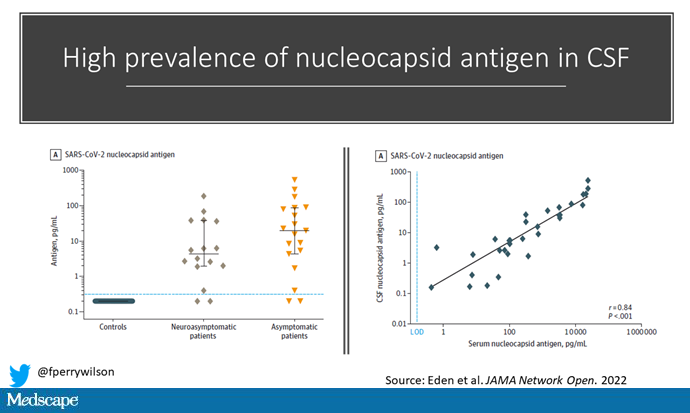
But virtually all patients, in both COVID groups, had SARS-CoV-2 nucleocapsid antigen, a structural protein of the virus, in the CSF. And the amount in the CSF was directly proportional to the amount in blood.
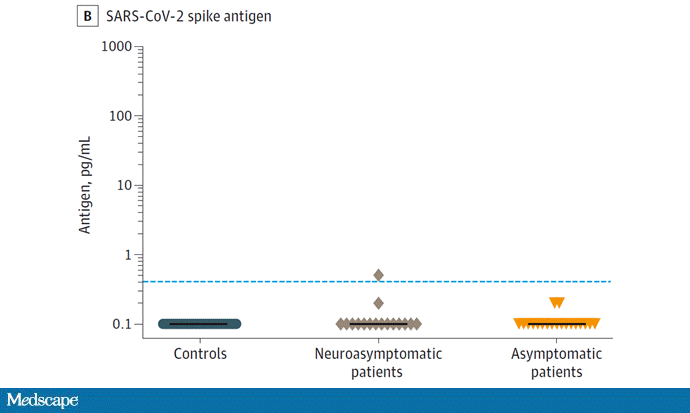
What that means is that pieces of the virus can pass through the blood-brain barrier, even if the whole virus itself cannot. Interestingly, only one patient with COVID had spike protein in the CSF, and that patient did not have neurologic symptoms.
But the presence of nucleocapsid antigen wasn’t different between COVID patients with and without neurologic symptoms. So what explains the symptoms?
Could it be the response to the antigen? The inflammation that the antigen triggers?
The authors looked at a variety of inflammatory biomarkers in the CSF. Compared with hospitalized controls — who had a spinal tap that ruled out infection — levels of interleukins 6 and 10, and interferon-gamma, were significantly higher.
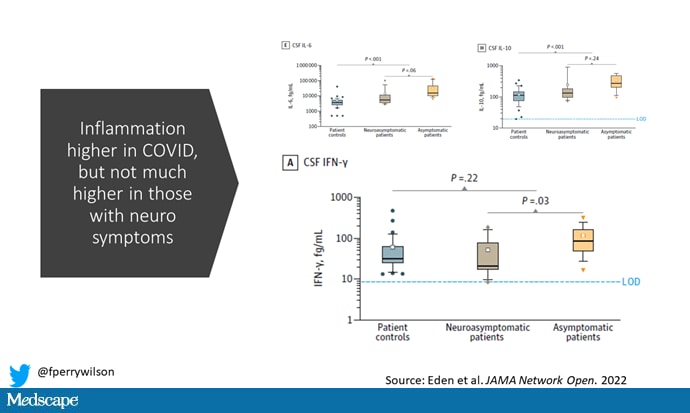
And though the levels of all of those markers trended higher in those who were neurosymptomatic, the differences aren’t dramatic, with the exception of interferon gamma. Of course, remember that those without neurologic symptoms were more likely to be given betamethasone than those with neurologic symptoms. It’s possible that’s why inflammation was a bit lower in those without symptoms.
So, is the case cracked? Have we discovered how COVID attacks the brain? Does COVID antigen slip through the blood-brain barrier, causing inflammation and all those neurologic symptoms? It’s a nice story, but I don’t think this study confirms it yet. A couple of things are clear. Evidence for direct infection is slim, for one. It’s also clear that COVID leads to inflammation, but the inflammation doesn’t seem to correlate well with symptoms.
Of course, the same amount of inflammation may affect different people differently, depending on the underlying substrate of the brain. It may be that some people can simply “handle” inflammation better than others. It’s not uncommon, for example, for individuals with mild dementia to become delirious in the hospital due to totally nonneurologic processes.
Or, as always with science, something else could be going on. That’s what makes this type of research so intriguing, so important, and so frustrating.
https://www.medscape.com/viewarticle/974300?src=soc_fb_220528_mscpedt_news_mdscp_brain&faf=1#vp_1
Créditos: Comité científico Covid