En atención a la creciente preocupación sobre la confianza en...
Leer más
Resurgence of avian influenza virus
Highly pathogenic avian influenza viruses (HPAIv) have recently been detected on the East coast of Canada (December 2021) and the United States (January 2022) and have been found in both wild birds and poultry (1). This comes after the same strain (known as H5N1) swept through Asia, Africa, and Europe in late 2021, replacing the previous HPAIv and causing widespread outbreaks and millions of deaths in poultry and wild birds. These HPAIv are of concern not only to birds but also to humans because they pose a potential pandemic risk. How has this virus emerged and spread so rapidly, and what does it mean for poultry, wild birds, and humans?
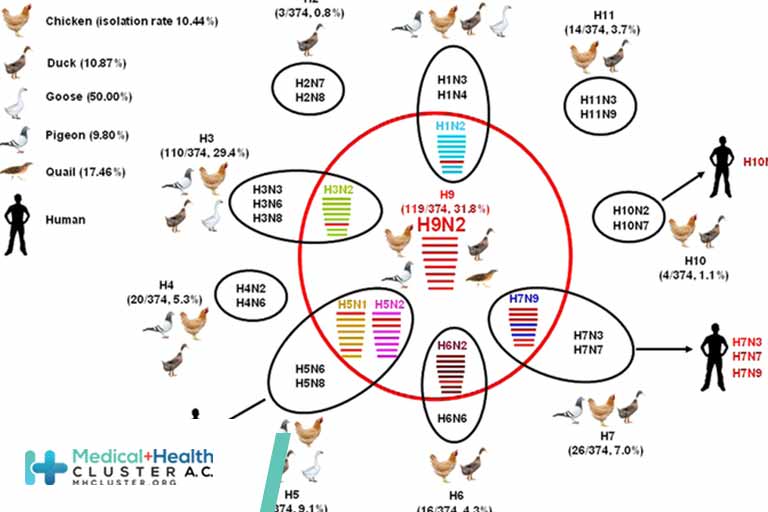
Influenza A viruses infect humans and a wide range of animal species such as pigs, poultry, and many wild birds, including waterbirds, the natural hosts of these viruses. Influenza A viruses are classified based on differences in their two most abundant surface proteins, hemagglutinin (H) and neuraminidase (N), of which there are 16 and 9 different subtypes, respectively, that infect avian species; these occur in different combinations, defining the virus (e.g., H5N1). Wild birds are infected with low-pathogenic avian influenza viruses (LPAIv), which they can carry asymptomatically. Only two H subtypes (H5 and H7) have repeatedly emerged as HPAIv to date, and these usually occur when LPAIv H5 and H7 viruses cross from wild birds into poultry, where changes in the H protein transform them into HPAIv, causing severe disease, devastating outbreaks, and up to 100% mortality in chickens (2). Although the N subtype may play some role in virus transmissibility, it does not determine disease severity.
The current circulating lineage of H5 HPAIv had its beginnings in Asia as early as 1996 as the goose/Guangdong lineage (gs/GD). After the emergence of a novel lineage and associated outbreaks in 2003, it spread to Asia, the Middle East, Africa, and Europe, where >400 million chickens, turkeys, and domestic ducks were culled and >600 human cases of H5N1 HPAIv were recorded within 5 years (3). These viruses became endemic in the poultry of many countries in Asia and Africa, with the gs/GD lineage diversifying into several genetic clades as a result of high infection rates, vaccination pressure, and circulation of this virus in an array of avian hosts. Since 2014, after evolution of the H gene, a new gs/GD lineage designated 2.3.4.4 has emerged, and these HPAIv have subsequently dominated outbreaks globally.
Why has the H5N1 subtype combination become globally dominant again? The reasons for the current 2021–2022 wave of H5 HPAIv are likely to be multifactorial. The reversion back to using N1 is probably serendipitous, but the current H5N1 virus clearly has a fitness advantage over the previous H5N6 or H5N8 HPAIv that predominated from 2014 to 2021. This has allowed H5N1 to rapidly displace other H5Nx viruses. Normally such a dramatic global sweep would be caused by a major change in the influenza H protein, but the H of the current H5N1 is similar to that of the previous H5N6 and H5N8 viruses, falling into the same genetic lineage (2.3.4.4). This leaves properties in the N1 or changes to other viral genes through reassortment or mutation as possible reasons for increased fitness. However, there may be other host factors leading to this spread, such as being able to infect a broader range of wild birds or reaching higher viral loads in birds, causing larger and more intense outbreaks. These matters need further, careful investigation.
How has the rapid spread of H5N1 HPAIv occurred? Although HPAIv often emerge in high-density poultry production systems, it is wild birds that can spread these viruses globally. The role of wild birds in spreading HPAIv H5 before 2014 was unclear. However, in late 2014, wild waterfowl spread HPAIv H5Nx from their breeding areas in Siberia to Europe and North America (4) and to Africa in 2017 along their established migratory flyways. Wild birds have now reintroduced H5 HPAIv into North America with detections in wild birds: great black-backed gulls (Larus marinus) in St. John’s Canada (November to December 2021) (4) and wild birds as well as backyard and commercial poultry flocks in the United States from January 2022 (1) (see the figure). H5Nx HPAIv have now been introduced into all continents except Australia, South America, and Antarctica, which have probably been spared because of ecological barriers to waterfowl migration from areas of endemic circulation; however, this situation could change.
What are the consequences of the H5N1 HPAIv spread? Although wild birds are able to spread these viruses through migration, the viruses may also cause their own mass mortality events. These mortality events in wild birds come with substantial conservation concern. For example, H5N1 HPAIv caused the death of hundreds of red knots (Calidris canutus) in the Netherlands in 2021 (5), 10,000 migratory common cranes (Grus grus) in Israel in December 2021 (6), ∼10% of the Svalbard breeding population of barnacle geese (Branta leucopsis) in late 2021 (7), and hundreds of Dalmatian pelicans (Pelecanus crispus) in northern Greece in 2022.
Outbreaks of H5Nx HPAIv have also had a substantial impact on poultry production and cost the sector billions of dollars since their emergence. Data reported to the World Organisation for Animal Health (OIE) found that between 2005 and 2019, there were 18,620 outbreaks in poultry reported across 76 countries. In 2020–2021 alone there have been more than 3000 HPAIv events reported (8), with ∼15,000,000 poultry losses (died or culled) globally as a result of H5Nx. The United Kingdom has experienced its biggest outbreak due to H5N1 HPAIv, with millions of poultry culled; there have also been 2804 outbreaks in Europe since October 2021 (up to 23 March 2022) (8, 9).
Onward transmission of HPAIv to humans is an ongoing threat that continues to be of pandemic concern. From 2003 to 2021, there have been 863 human cases of H5N1 HPAIv, resulting in 456 deaths reported to the World Health Organization (WHO), with virtually all of these cases occurring before 2016. Although this earlier “classic” strain of H5N1 caused severe infections in more than half of those infected, the number of people infected was relatively low given that millions of birds and hundreds of thousands of poultry workers, farmers, and live-bird market-stall holders were in direct contact with infected birds. Furthermore, these infections were almost exclusively associated with contact with infected birds, with no sustained onward human-to-human transmission detected, confirming that these viruses were not well-enough adapted to humans to be a major concern. The more recent 2.3.4.4 H5 HPAIv have produced similarly low rates of human infections, possibly because these viruses share the same ancestral gs/GD lineage. However, different pathogenicity has been observed when human H5 infections do occur, with the earlier H5N1 and H5N6 HPAIv appearing more severe and causing more deaths in humans than H5N8 viruses. Notably, all these H5Nx HPAIv strains remain highly transmissible and deadly to poultry and, to a lesser extent, wild birds.
H5N8 2.3.4.4 HPAIv have resulted in very few human cases despite their high circulation from 2014 to 2021. Several mild H5N8 infections were detected in December 2020 in poultry workers in Astrakhan Oblast (Russian Federation), none of whom required hospitalization (10). Three human infections with H5N? HPAIv (probably N1) were reported in Nigeria in March 2021, but it is unclear if these were true infections or environmental carriage of virus because all cases were asymptomatic. By contrast, between 2014 and 16 March 2022, H5N6 has caused 77 human infections with 32 deaths, with all but one case occurring in China. Of recent concern has been the apparent increase in H5N6 HPAIv human cases in China in 2021, where 33 cases (out of 76 total cases) with 11 deaths were reported, along with a further 17 cases with at least five deaths in 2022 [up to 16 March 2022 (11)]. These recently increased numbers may be due to enhanced respiratory and pneumonia surveillance during the COVID-19 pandemic, but the situation needs to be closely monitored. Reassuringly, no onward human-to-human transmission has been detected from any of these H5N6 or H5N8 HPAIv infections. To date, only a single human case with the recent 2.3.4.4 H5N1 HPAIv has been reported—a 79-year-old man in the United Kingdom who was infected from local ducks in mid-December 2021 but who remained asymptomatic (12).
What would raise the concern for H5N1 HPAIv for humans? A recent European assessment (13) determined that the risk of infection with H5Nx for the general population in Europe was low, and for occupationally exposed people, the risk was low to medium (but with high uncertainty) (14). Further adaption would need to occur in this current virus to increase its ability to transmit between humans efficiently, a process that is only partially understood; although this has not occurred yet, the persistence of H5Nx HPAIv increases the likelihood. As with COVID-19, if this adaption occurred and the virus became efficient at airborne transmission between humans, it would be virtually impossible to control.

OPEN IN VIEWER
What can be done to curb the H5N1 HPAIv threat? Although H5N1 and H5Nx HPAIv are, at present, a low threat to humans, it is early in the outbreak and each potential pandemic threat should be taken seriously. To gauge the risk, international organizations such as WHO, OIE, and the Food and Agriculture Organization of the United Nations (FAO) all have programs to investigate HPAIv in humans, poultry, and wild birds. Furthermore, continued investment in surveillance of wild birds and poultry and of humans at the human-poultry interface are critical. To mitigate the potential pandemic threat from H5Nx viruses, WHO continually prepares a stock of those viruses (and others) that are considered to be potentially dangerous to humans, which can be rapidly accessed for vaccine manufacture if required. Effective H5 HPAIv vaccines are also important in protecting poultry, and their use will reduce spillover into wild birds and humans. In 2017, mass poultry vaccination with a combined H5 and H7 vaccine was successful in controlling H7N9 poultry outbreaks and human infections in China. After mass vaccination and the closure of live-bird markets, H7N9 human infections dropped from 759 (with 281 deaths) in 2017 to only two cases in 2018 (15). Notably, countries that do not use poultry influenza vaccines and instead rely on the culling of infected birds to control HPAIv outbreaks may now consider the implementation of a vaccination program, given the impact of the current H5N1 outbreak. Additionally, measures such as reduction of flock size and density and avoidance of poultry production in waterbird-rich areas have been proposed to prevent spillovers of HPAIv into wild birds. The ongoing 2021–2022 wave of avian influenza H5N1 is unprecedented in its rapid spread and extremely high frequency of outbreaks in poultry and wild birds and is a continuing potential threat to humans.
Créditos: Comité científico Covid




