En atención a la creciente preocupación sobre la confianza en...
Leer más
Effect of Antiplatelet Therapy on Survival and Organ Support–Free Days in Critically Ill Patients With COVID-19
Question Does antiplatelet therapy administered to critically ill patients with COVID-19 improve organ support–free days (a composite end point of in-hospital mortality and duration of intensive care unit–based respiratory or cardiovascular support) up to day 21?
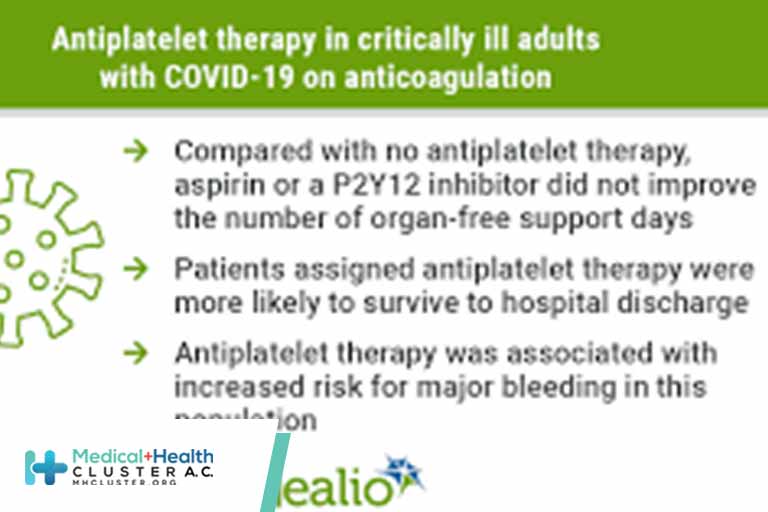
Findings In this bayesian randomized clinical trial that included 1557 patients, antiplatelet therapy with either aspirin or a P2Y12 inhibitor, compared with no antiplatelet therapy, resulted in a 95.7% posterior probability of futility with regard to the odds of improvement in organ support–free days within 21 days.
Meaning Among critically ill patients with COVID-19, there was a low likelihood that treatment with an antiplatelet agent provided improvement in organ support–free days within 21 days.
Importance The efficacy of antiplatelet therapy in critically ill patients with COVID-19 is uncertain.
Objective To determine whether antiplatelet therapy improves outcomes for critically ill adults with COVID-19.
Design, Setting, and Participants In an ongoing adaptive platform trial (REMAP-CAP) testing multiple interventions within multiple therapeutic domains, 1557 critically ill adult patients with COVID-19 were enrolled between October 30, 2020, and June 23, 2021, from 105 sites in 8 countries and followed up for 90 days (final follow-up date: July 26, 2021).
Interventions Patients were randomized to receive either open-label aspirin (n = 565), a P2Y12 inhibitor (n = 455), or no antiplatelet therapy (control; n = 529). Interventions were continued in the hospital for a maximum of 14 days and were in addition to anticoagulation thromboprophylaxis.
Main Outcomes and Measures The primary end point was organ support–free days (days alive and free of intensive care unit–based respiratory or cardiovascular organ support) within 21 days, ranging from −1 for any death in hospital (censored at 90 days) to 22 for survivors with no organ support. There were 13 secondary outcomes, including survival to discharge and major bleeding to 14 days. The primary analysis was a bayesian cumulative logistic model. An odds ratio (OR) greater than 1 represented improved survival, more organ support–free days, or both. Efficacy was defined as greater than 99% posterior probability of an OR greater than 1. Futility was defined as greater than 95% posterior probability of an OR less than 1.2 vs control. Intervention equivalence was defined as greater than 90% probability that the OR (compared with each other) was between 1/1.2 and 1.2 for 2 noncontrol interventions.
Results The aspirin and P2Y12 inhibitor groups met the predefined criteria for equivalence at an adaptive analysis and were statistically pooled for further analysis. Enrollment was discontinued after the prespecified criterion for futility was met for the pooled antiplatelet group compared with control. Among the 1557 critically ill patients randomized, 8 patients withdrew consent and 1549 completed the trial (median age, 57 years; 521 [33.6%] female). The median for organ support–free days was 7 (IQR, −1 to 16) in both the antiplatelet and control groups (median-adjusted OR, 1.02 [95% credible interval {CrI}, 0.86-1.23]; 95.7% posterior probability of futility). The proportions of patients surviving to hospital discharge were 71.5% (723/1011) and 67.9% (354/521) in the antiplatelet and control groups, respectively (median-adjusted OR, 1.27 [95% CrI, 0.99-1.62]; adjusted absolute difference, 5% [95% CrI, −0.2% to 9.5%]; 97% posterior probability of efficacy). Among survivors, the median for organ support–free days was 14 in both groups. Major bleeding occurred in 2.1% and 0.4% of patients in the antiplatelet and control groups (adjusted OR, 2.97 [95% CrI, 1.23-8.28]; adjusted absolute risk increase, 0.8% [95% CrI, 0.1%-2.7%]; 99.4% probability of harm).
Conclusions and Relevance Among critically ill patients with COVID-19, treatment with an antiplatelet agent, compared with no antiplatelet agent, had a low likelihood of providing improvement in the number of organ support–free days within 21 days.
Trial Registration ClinicalTrials.gov Identifier: NCT02735707
Thrombotic events are common in patients hospitalized with COVID-19 and occur in spite of standard thromboprophylaxis, with critically ill patients being at highest risk.1-7 Thrombotic events have been reported in the venous, arterial, and microvascular circulations and are independently associated with poor outcomes.4 Vascular endothelial injury and inflammation activate intravascular coagulation through diverse mediators such as elevated fibrinogen, factor VIII, von Willebrand factor, platelet activation, impaired fibrinolysis, and reduced antithrombin.8
In a collaborative multiplatform trial that included the Randomized, Embedded, Multifactorial Adaptive Platform Trial for Community-Acquired Pneumonia (REMAP-CAP), therapeutic-dose heparin was found to improve organ support–free days in non–critically ill patients,9 but not in critically ill patients,10 hospitalized for COVID-19. Accordingly, despite a high occurrence of thrombosis, optimal antithrombotic strategies in critically ill patients remain unknown. Platelet activation has been implicated in the COVID-19 inflammatory response,11,12 and autopsies have shown microvascular thrombi with megakaryocyte and platelet-fibrin deposition in the setting of organ failure.13-15 In this trial, the effect of antiplatelet therapy (aspirin or P2Y12 inhibitor) on the composite of hospital survival and organ support provision for up to 21 days was evaluated in patients hospitalized with COVID-19.
REMAP-CAP is an international, adaptive platform trial designed to iteratively determine best treatment strategies for patients with severe pneumonia in both pandemic and nonpandemic settings, and has reported on corticosteroids, anticoagulants, antivirals, interleukin 6 receptor antagonists, and convalescent plasma in patients with COVID-19.9,10,16-19 Patients eligible for the platform are assessed for eligibility and potentially randomized to 1 or more interventions across multiple domains. Domains encompass therapeutic areas and contain 2 or more interventions (including control). Details of the trial design have been reported previously20 and are available in the trial protocol and statistical analysis plan (Supplement 1). The trial was approved by relevant regional ethics committees and conducted in accordance with Good Clinical Practice guidelines and the principles of the Declaration of Helsinki.21 Written or oral informed consent, in accordance with regional legislation, was obtained from all patients or their surrogates. To account for the observed racial and ethnic differences in outcomes during the pandemic, this trial collected self-reported race and ethnicity data from either the participants or their surrogates via fixed categories appropriate to their region.
Patients admitted to the hospital, aged 18 years or older, with clinically suspected or microbiologically confirmed COVID-19 were eligible for enrollment. Patients admitted to an intensive care unit (ICU) and receiving respiratory or cardiovascular organ support were classified as critically ill and all others as non–critically ill. Respiratory organ support was defined as invasive or noninvasive mechanical ventilation including via high-flow nasal cannula if the flow rate was at least 30 L/min and the fraction of inspired oxygen was at least 0.4. Cardiovascular organ support was defined as receipt of vasopressors or inotropes. Exclusion criteria included presumption that death was imminent with lack of commitment to full support, clinical or laboratory-based bleeding risk sufficient to contraindicate antiplatelet therapy, creatinine clearance less than 30 mL/min or receipt of kidney replacement therapy, enrollment in an external trial of anticoagulation or antiplatelet therapy, or enrollment in the anticoagulation domain of the trial platform for participants older than 75 years. Patients were also excluded if they were already receiving antiplatelet therapy or nonsteroidal anti-inflammatory drugs (NSAIDs), if a clinical decision had been made to commence antiplatelet or NSAID therapy, or if a treating clinician believed that participation in the domain would not be in the best interests of a patient. Critically ill patients had to be enrolled within 48 hours of admission to an ICU. Patients were enrolled from 105 sites in 8 countries (Canada, France, Germany, India, Italy, Nepal, the Netherlands, and the United Kingdom). Additional platform and antiplatelet domain–specific exclusion criteria are listed in eAppendix 1 in Supplement 2.
The antiplatelet domain included 3 groups to which patients could be assigned: aspirin, P2Y12 inhibitor, and no antiplatelet therapy (control). Each site’s clinical investigator team chose a priori at least 2 intervention groups, one of which had to be control, to which patients could be randomized. Sites that chose the P2Y12 inhibitor intervention further selected which P2Y12 inhibitor would be administered at their site (clopidogrel, prasugrel, or ticagrelor) according to availability and local preference. Patients were randomized via centralized computer program with allocation ratios dependent on the number of interventions at each site. Patients were initially randomized equally across the interventions available at each site. The domain also permitted variation in allocation ratios based on regular adaptive analysis. Randomization started on October 30, 2020. Response-adaptive randomization was applied on April 21, 2021 (see eFigure 1 in Supplement 2 for recruitment rates over time). Patients could be randomized to additional interventions within other domains, depending on domains active at the site, patient eligibility, and consent (see http://www.remapcap.org). Other aspects of care were provided per each site’s standard care.
All antiplatelet interventions were administered enterally until study day 14 or hospital discharge, whichever occurred first. After 14 days, decisions regarding antiplatelet therapy were at the discretion of treating clinicians. Antiplatelet dosing was as follows: aspirin, 75 to 100 mg once daily; clopidogrel, 75 mg once daily without a loading dose; ticagrelor, 60 mg twice daily without a loading dose; prasugrel, a 60-mg loading dose followed by 10 mg daily (if aged <75 years and weight ≥60 kg) or 5 mg daily (if aged ≥75 years or weight <60 kg). Gastric acid suppression was recommended for patients receiving antiplatelet therapy through co-administration of either proton pump inhibitor or H2 receptor antagonist. Antiplatelet therapy could be discontinued if there was an adverse event or commenced in the control group if clinically warranted for a standard indication other than COVID-19. Patients received concurrent anticoagulation thromboprophylaxis according to standard care if not randomized in the anticoagulation domain of the trial.
The primary outcome was respiratory and cardiovascular organ support–free days to day 21. In this composite ordinal outcome, all deaths occurring during the index hospitalization were assigned the worst possible outcome (–1). Among survivors, respiratory and cardiovascular organ support–free days were calculated up to day 21 (survivors with no organ support were assigned a score of 22). Secondary outcomes were survival to day 90, progression to invasive mechanical ventilation, extracorporeal membrane oxygenation or death among those not receiving that support at baseline, vasopressor-/inotrope-free days, respiratory support–free days, duration of ICU stay, duration of hospital stay, serious adverse events, World Health Organization ordinal score for clinical improvement (ranging from 0 [no evidence of infection] to 8 [death]), major bleeding up to day 14 defined according to International Society of Hemostasis and Thrombosis criteria (see eAppendix 1 in Supplement 2 for details) including fatal and intracranial bleeding, venous thromboembolism (deep vein thrombosis, pulmonary embolism, and other venous thromboembolism), arterial thrombosis (cerebrovascular event, myocardial infarction, and other arterial thrombotic event), as well as a composite of thrombosis or death. Individual components of the above mentioned composite outcomes were also prespecified as secondary outcomes but are not analyzed individually in this report. Thrombotic outcomes and major bleeding events were centrally adjudicated in a blinded manner.
The trial was designed with no maximum sample size given the uncertainty of the pandemic. Sample size calculations for the primary outcome were performed using trial simulations of the adaptive design rules (see eFigure 2 in Supplement 2). The domain had at least 90% power to demonstrate superiority of an antiplatelet therapy to no antiplatelet therapy with 900 patients enrolled assuming an odds ratio effect size of 1.5. The cumulative type I error rate up to 3000 patients was less than 5%.
The primary analysis was a bayesian cumulative logistic model, which calculated posterior probability distributions of organ support–free days (primary outcome) based on evidence accumulated in the trial and prior information. Prior distributions for treatment effects in critically and non–critically ill patients were nested in a hierarchical prior distribution centered on an overall intervention effect estimated with a neutral prior assuming no treatment effect (standard normal prior on the log odds ratio; see eFigure 2 in Supplement 2). The primary model estimated treatment effects for each intervention within each domain and prespecified treatment-by-treatment interactions. The primary model also adjusted for location (site nested within country), age (categorized into 6 groups), sex, and time period (2-week epochs). The model was fit using a Markov chain Monte Carlo algorithm that calculated the posterior distribution of the proportional odds ratios, including medians and 95% credible intervals (CrIs). The predefined statistical triggers for trial conclusions were (1) a superiority conclusion if there was greater than 99% posterior probability that an intervention was optimal compared with all other interventions; (2) an inferiority conclusion if there was less than 1% posterior probability that an intervention was optimal; (3) intervention efficacy if there was greater than 99% posterior probability that the odds ratio was greater than 1 compared with control; (4) intervention futility if there was greater than 95% posterior probability that the odds ratio was less than 1.2 compared with control; or (5) intervention equivalence if there was greater than 90% probability that the odds ratio (compared with each other) was between 1/1.2 and 1.2 for 2 noncontrol interventions.
On March 22, 2021, the equivalence trigger was reached for the primary outcome in critically ill patients for the aspirin and P2Y12 inhibitor groups. Randomization continued for these 2 antiplatelet groups, but for critically ill patients, the groups were statistically pooled and a single treatment effect relative to control was estimated for subsequent primary analysis. The 2 antiplatelet groups were not pooled for non–critically ill patients as no equivalence threshold had been reached. A prespecified interaction was modeled between antiplatelet therapy and therapeutic-dose heparin in the anticoagulation domain of the trial.
The primary analysis was conducted by an independent statistical analysis committee including all patients with COVID-19 randomized to any domain up to June 23, 2021 (and with complete follow-up for the primary outcome). Patients were analyzed in the groups to which they were originally randomized. There was no imputation of missing data for primary or secondary outcomes. Recruitment of non–critically ill patients was stopped due to slow recruitment and external evidence even though no statistical threshold for the primary outcome had been reached. The analysis of the results for non–critically ill patients is presented in eTables 2-4 in Supplement 2 for completeness.
Not all patients enrolled in the platform were eligible for all domains or interventions (dependent on active domains/interventions at the site, eligibility criteria, and patient/surrogate consent). Therefore, the analytical model included covariate terms reflecting randomization to each domain and the site, so that treatment effects were estimated only from patients who were concurrently randomized within the domain and directly comparing specific interventions available at each site. Patients enrolled outside the antiplatelet domain did not contribute to estimates of antiplatelet treatment effect but did contribute to the estimates of the covariate effects, providing the most robust estimation of covariate effects.16,20
Sensitivity and secondary analyses were performed by investigators blinded to ongoing interventions, so these analyses were restricted to data from patients enrolled in domains that were unblinded at the time of analysis with no adjustment for assignment in the ongoing domains. Treatment effects were also analyzed for aspirin and P2Y12 inhibitors compared with control separately. Prespecified sensitivity analyses included removing time and site effects from the model, as well as independent priors for the 2 antiplatelet treatments and alternative priors for interactions with other interventions. Secondary dichotomous outcomes were analyzed with bayesian logistic regression models. The secondary time-to-event outcomes (mortality and length of stay) were analyzed using a piecewise exponential bayesian model to estimate hazard ratio effects. No formal hypothesis tests were performed on secondary outcomes, and summaries of the posterior distributions and probabilities are provided for descriptive purposes only. Prespecified subgroup analyses included baseline mechanical ventilation status, age category (<50, 50-70, or ≥70 years), and baseline anticoagulation dose (defined in eTable 1 in Supplement 2). In a post hoc analysis, the baseline anticoagulation categories were collapsed into 2 categories, therapeutic dose and less than therapeutic dose. If the dose was not recorded, it was included in an unknown-dose category. Further details of all analyses are provided in eAppendix 1 in Supplement 2 and in the statistical analysis plan (Supplement 1). Data management and summaries were created using R version 3.6.0; the primary analysis was computed in R version 4.0.0 using the rstan package version 2.21.1. Additional data management and analyses were performed in SQL 2016, SPSS version 26, and Stata version 14.2.
Créditos: Comité científico Covid




