En atención a la creciente preocupación sobre la confianza en...
Leer más
The Seven Symptoms That Best Predict COVID

Welcome to Impact Factor, your weekly dose of commentary on a new medical study. I’m Dr. F. Perry Wilson of the Yale School of Medicine.
This week, we’re going to talk about COVID symptoms. I know — we’re almost 2 years into this pandemic; why do we need to talk about symptoms now? The short answer is because testing isn’t ubiquitous enough. We need to know what symptoms are sensitive and specific for COVID in order to know who should be tested or potentially isolated. And with respiratory virus season around the corner, identifying COVID-specific symptoms is more important than ever.
One problem with figuring out what symptoms are seen in COVID is that most studies look at people who test positive for COVID, and most people get tested when they have symptoms.
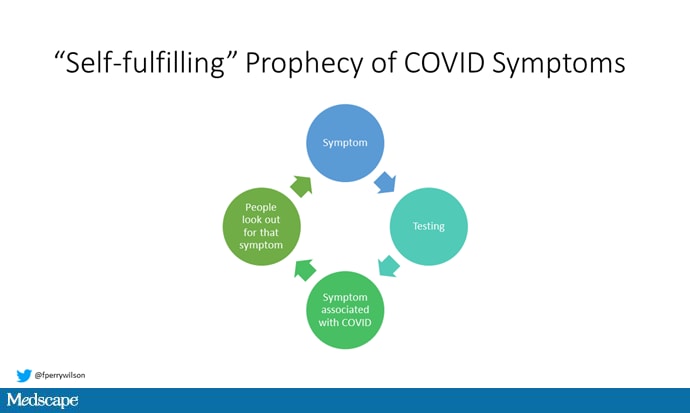
This means certain symptoms might become an almost self-fulfilling prophecy. The only way around this is to do random, population-based screening for COVID, and that is exactly what this paper, appearing in PLOS Medicine, does.
Throughout the pandemic, the National Health Service in England has been doing random COVID prevalence surveys throughout the country, testing a subset of their population regardless of symptom status, to figure out where the disease is and where it is going. I know — it must be nice, right? This particular paper looks at successive samples during the first “wild-type” surge of cases in England and then the subsequent alpha variant outbreak.
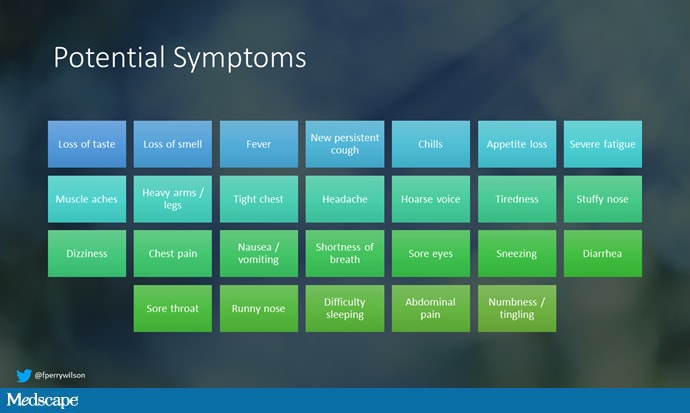
Participants completed a survey reporting symptoms over the past 4 weeks and the list was broad, as you can see.
Then, a PCR test was performed.
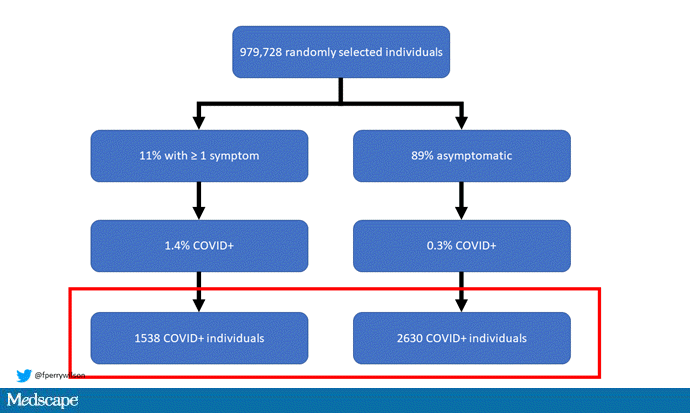
Now, since this was a general population sample, you won’t be surprised to see that the positivity rate was pretty low; just around 4000 individuals out of 1 million tested positive. And the presence of any of these symptoms was strongly associated with COVID-19.
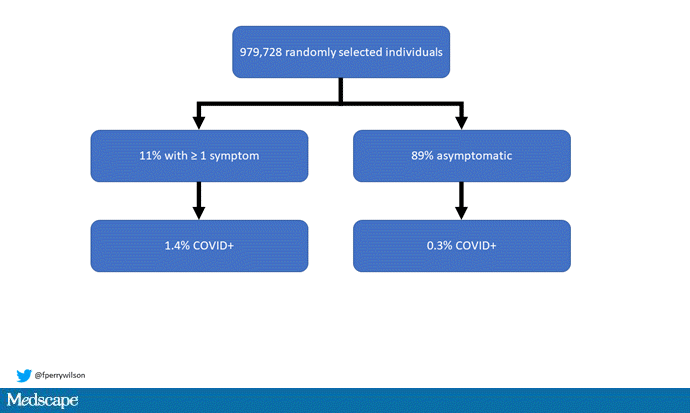
But the math here is quirky. Since symptoms are rare in the general population, the majority of the COVID cases were actually in asymptomatic people.
The take-home here is that asymptomatic (or at least presymptomatic) COVID is real and common. But also that symptoms still make it more likely that you actually have COVID.
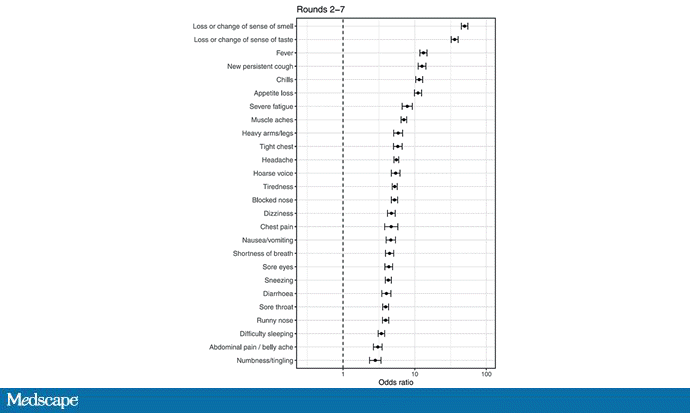
But this is any symptom. The paper breaks down the whole panoply of potential symptoms to see which are more strongly associated with COVID than others. All of the symptoms on the list made COVID more likely, but this figure shows which were most strongly associated.
Créditos: Comité científico Covid