En atención a la creciente preocupación sobre la confianza en...
Leer más
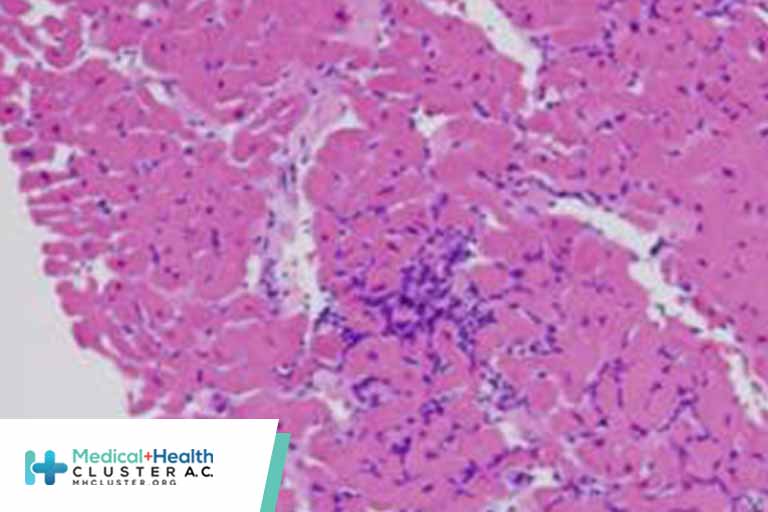
Myocarditis
Practice Essentials
Myocarditis is an inflammatory disease of the myocardium with a wide range of clinical presentations, from subtle to devastating.
The image below depicts numerous lymphocytes with associated myocyte damage.
Signs and symptoms
Myocarditis usually manifests in an otherwise healthy person and can result in rapidly progressive heart failure and arrhythmia. Patients with myocarditis have a clinical history of acute decompensation of heart failure, but they have no other underlying cardiac dysfunction or have low cardiac risk.
Patients with myocarditis may present with the following signs and symptoms:
-
Mild symptoms of chest pain (in concurrent pericarditis), fever, sweats, chills, dyspnea
-
In viral myocarditis: Recent history (≤1-2 wk) of flulike symptoms of fevers, arthralgias, and malaise or pharyngitis, tonsillitis, or upper respiratory tract infection
-
Palpitations, syncope, or sudden cardiac death due to underlying ventricular arrhythmias or atrioventricular block (especially in giant cell myocarditis)
-
Heart failure
See Clinical Presentation for more detail.
Diagnosis
The diagnosis of acute myocarditis is usually presumptive, based on patient demographics and the clinical course. Because many cases of myocarditis are not clinically obvious, a high degree of suspicion is required.
Patients with myocarditis usually present with signs and symptoms of acute decompensation of heart failure (eg, tachycardia, gallop, mitral regurgitation, edema) and, in those with concomitant pericarditis, with pericardial friction rub.
Specific findings in special cases are as follows:
-
Sarcoid myocarditis: Lymphadenopathy, also with arrhythmias, sarcoid involvement in other organs (up to 70%)
-
Acute rheumatic fever: Usually affects heart in 50-90%; associated signs, such as erythema marginatum, polyarthralgia, chorea, subcutaneous nodules (Jones criteria)
-
Hypersensitive/eosinophilic myocarditis: Pruritic maculopapular rash and history of using offending drug
-
Giant cell myocarditis: Sustained ventricular tachycardia in rapidly progressive heart failure [1]
-
Peripartum cardiomyopathy: Heart failure developing in the last month of pregnancy or within 5 months following delivery
Testing
Laboratory studies use to evaluate suspected myocarditis may include the following:
-
Complete blood count
-
Erythrocyte sedimentation rate level (and that of other acute phase reactants [eg, C-reactive protein])
-
Rheumatologic screening
-
Cardiac enzyme levels (eg, creatine kinase or cardiac troponins)
-
Serum viral antibody titers
-
Viral genome testing in endomyocardial biopsy
-
Electrocardiography
Imaging studies
The following imaging studies may be used to assess patients with suspected myocarditis:
-
Echocardiography: To exclude other causes of heart failure (eg, amyloidosis or valvular or congenital causes) and to evaluate the degree of cardiac dysfunction
-
Antimyosin scintigraphy: To identify myocardial inflammation
-
Coronary angiography: To rule out coronary ischemia as cause of new-onset heart failure
-
Gadolinium-enhanced magnetic resonance imaging: To assess extent of inflammation and cellular edema; nonspecific
Procedures
Endomyocardial biopsy is the standard tool for diagnosing myocarditis. However, the use of routine endomyocardial biopsy in establishing the diagnosis of myocarditis rarely is helpful clinically, since histologic diagnosis seldom has an impact on therapeutic strategies, unless giant cell myocarditis is suspected. [2, 3]
The Heart Failure Society of America 2010 comprehensive heart failure practice guideline recommends considering endomyocardial biopsy for patients with acute deterioration of heart function of unknown origin that is not responding to medical treatment. [4]
See Workup for more detail.
Management
In general, treatment of either acute or chronic myocarditis is aimed at reducing congestion and improving cardiac hemodynamics in heart failure, as well as providing supportive therapy, with the hope of prolonging survival. Treatment of heart failure follows the same treatment regimen regardless of the underlying cause (ie, inhibitors, beta-adrenergic blockers).
Pharmacotherapy
Medications used in the management of myocarditis include the following:
-
Vasodilators (eg, nitroglycerin, sodium nitroprusside)
-
Angiotensin-converting enzyme inhibitors (eg, enalapril)
-
Diuretics (eg, furosemide)
Anticoagulation when there is definte indication such as atrial fibrillation or intracardiac thrombus.
Antiarrhythmics can be used cautiously, although most antiarrhythmic drugs have negative inotropic effects that may aggravate heart failure. (Supraventricular arrhythmias should be converted electrically.) High-grade ventricular ectopy and ventricular tachyarrhythmia should be treated cautiously with beta blockers and antiarrhythmics.
Inotropic drugs (eg, dobutamine, milrinone) may be necessary for severe decompensation, although they are highly arrhythmogenic. Long-term treatment follows the same medical regimen, including angiotensin-converting enzyme inhibitors, beta blockers, and aldosterone receptor antagonists. However, in some instances, some of these drugs cannot be implemented initially because of hemodynamic instability.
Nonpharmacotherapy
Supportive care in patients with myocarditis includes the following:
-
Hemodynamic and cardiac monitoring
-
Administration of supplemental oxygen
-
Fluid management
Surgical option
Surgical intervention in myocarditis may include the following:
-
Temporary transvenous pacing for complete heart block
-
Cardiac transplantation
-
Extreme cases: Ventricular assist device or percutaneous circulatory support; left ventricular assistive devices (LVADs) and extracorporeal membrane oxygenation [5]
See Treatment and Medication for more detail.
Créditos: Comité científico Covid




