En atención a la creciente preocupación sobre la confianza en...
Leer más
Lessons Learned About Aerosol Drug Delivery in the Era of COVID‑19
Reasonable concerns exist regarding the transmission risk of COVID-19 due to aerosol dispersion. This article provides clarity on lessons learned during the COVID-19 pandemic and summarizes strategies based on the best available evidence
esson 1: The risk of device contamination and viral transmission differs between devices.
Inhalers generate less aerosol mass due to lower emitted doses and have a short treatment time.1 The drug is also enclosed in inhalers. According to expert opinion, device contamination and viral transmission with inhalers are less than with nebulizers that require extensive cleaning after a long treatment time.1 While there is no original study comparing different nebulizers on device contamination and viral transmission, mesh nebulizers may be less prone to device contamination than jet nebulizers because they separate the drug from the patient interface, operate with electricity/battery, and have a small residual volume (Figure 1).1
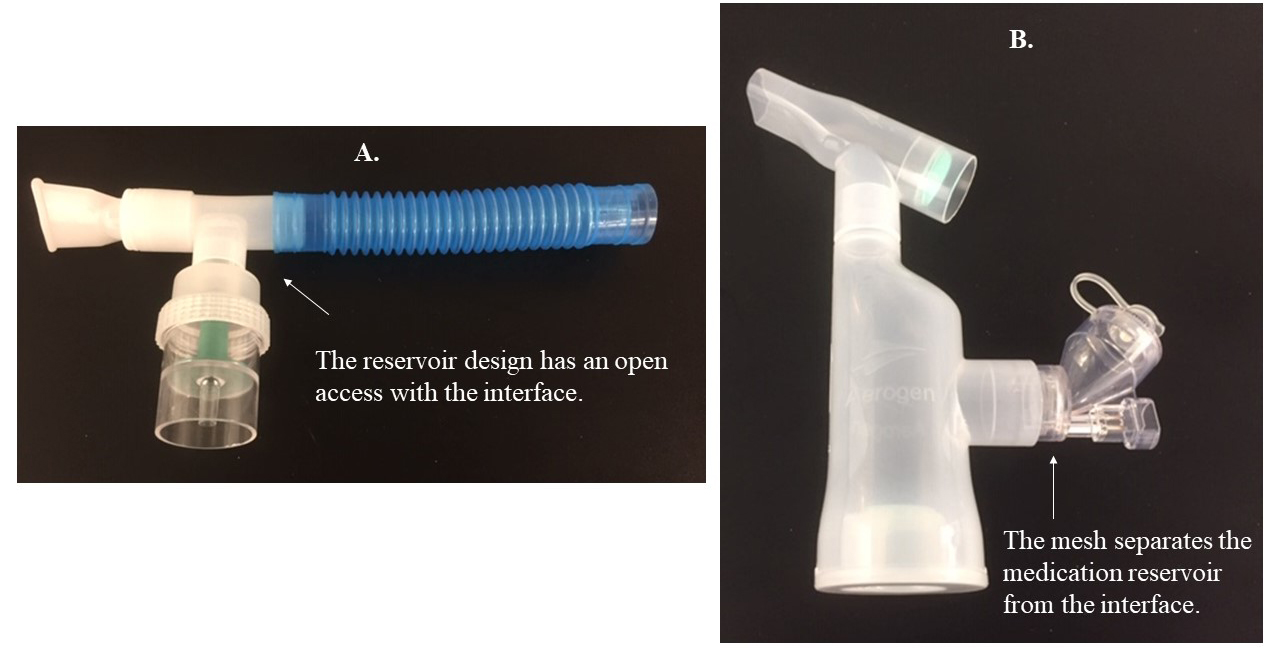
Jet nebulizers have an open medication reservoir, positioned below the gas pathway/circuit, in which infected condensate may drop into the reservoir and contaminate the jet nebulizer.1,2 The large residual volume of jet nebulizers may create a hospitable environment for pathogens when not cleaned between treatments.1,2 Also, jet nebulizers operate with an external gas flow that increases exhaled aerosol dispersion to the environment.3 Attaching a filter to the expiratory outlet of nebulizers effectively captures exhaled aerosol droplets during therapy,4,5 but evaluating the efficiency of these filters in preventing viral transmission is warranted.1,6
Lesson 2: Select an aerosol device based on the patient’s clinical status.
While inhalers are good options for spontaneously breathing patients without comorbidities, nebulizers should be used in patients who cannot perform the optimum breathing technique required by inhalers, or when the drug formulation is unavailable as an inhaler.1,6,7
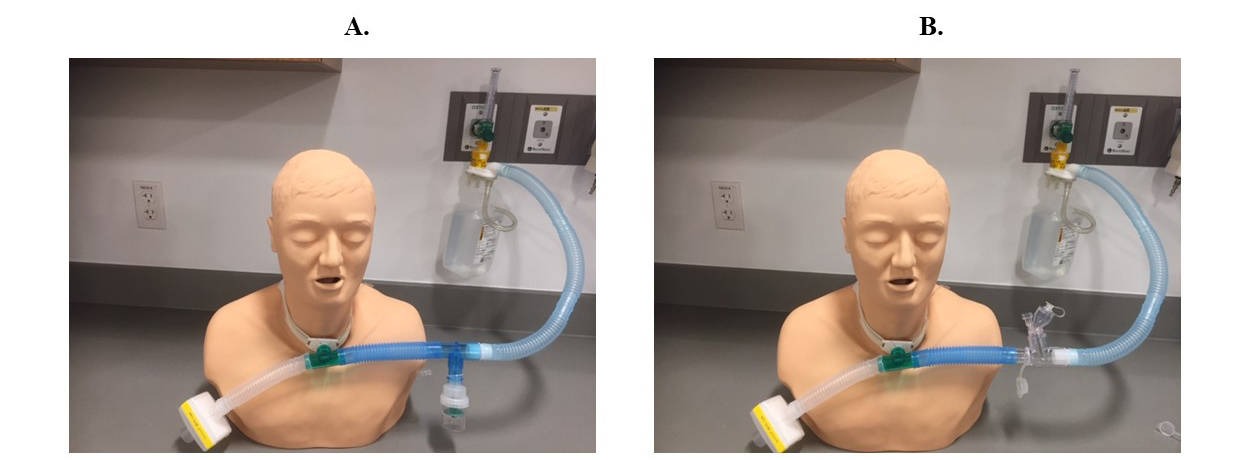
In patients receiving high-flow nasal cannula (HFNC) oxygenation, or noninvasive ventilation or mechanical ventilation, clinicians should use jet nebulizers with a valved T-piece or mesh nebulizers to avoid breaking the circuit for device placement.1,6,8 Keeping the circuit intact and attaching a HEPA filter to the ventilator expiratory outlet is essential to prevent viral transmission.1,6 Since connecting pressurized metered-dose inhalers directly to the tracheotomy tube will cause cough and airway irritation, jet nebulizers with a valved T-piece or mesh nebulizers should be attached to the circuit of the high-flow oxygen device to keep the circuit intact and prevent viral transmission during aerosol therapy (Figure 2).9
Lesson 3: Aerosols can be delivered through HFNC.
Concerns remain for exhaled air dispersion and viral transmission with HFNC. However, the dispersion distance of exhaled particles with HFNC is less than with Venturi and nonrebreather masks.10,11 Bacterial growth in air samples between HFNC and the simple mask does not differ significantly.12 Additionally, HFNC does not seem to increase the risk of infection via droplets.13 Due to the efficacy of HFNC in hypoxemic respiratory failure, potentially limited numbers of ventilators, and risk with early intubations, clinicians should weigh benefits against harms and consider delivering aerosolized medications through HFNC by implementing the strategies listed in Table 1.8
Lesson 4: Interface selection is as important as device selection in COVID-19.
Using face masks and tracheostomy masks increases exhaled aerosol dispersion to the environment because of open aperture and a loose fit.9,14 Instead, use a mouthpiece or T-piece for aerosol delivery to spontaneously breathing or tracheotomized patients, respectively.5,6,9
Lesson 5: Reduce exhaled aerosol dispersion to the environment through good infection control and prevention.
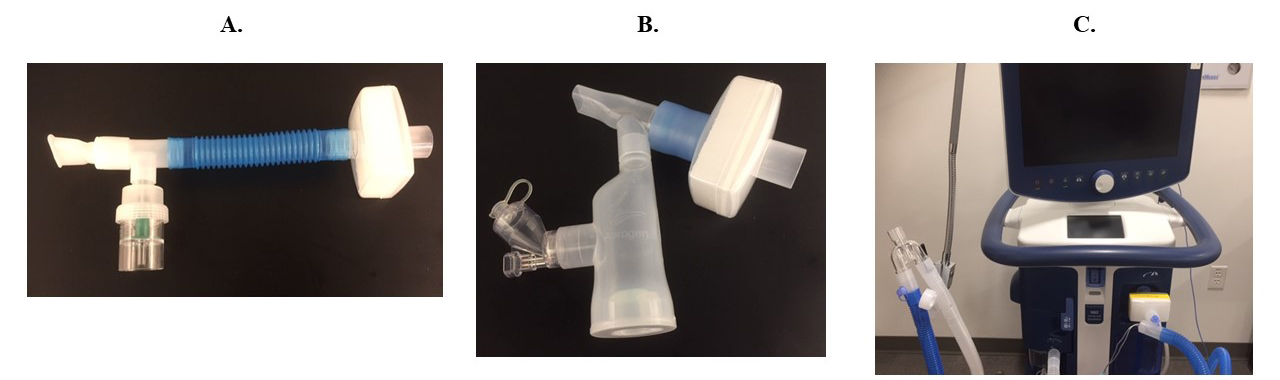
Using a mouthpiece, attaching filters to the expiratory outlet of nebulizers and ventilators (Figure 3) and placing a surgical mask over HFNC decreases exhaled aerosol dispersion.1,5,6,8,15-17
Patients should wear masks when possible, and use tissues during a cough or sneeze.16 Aseptic technique is vital during device preparation, cleaning, and maintenance.1 Clinicians should isolate patients in negative pressure rooms, adhere to airborne precautions, stringently use personal protective equipment, and bundle activities to minimize room entries in the era of COVID-19.1,6
Table 1. Strategies for Safe and Effective Delivery of Aerosolized Medications to Different Patient Populations
| Spontaneous Breathing | High-Flow Nasal Cannula | Mechanical Ventilation | Tracheostomy |
|---|---|---|---|
| Avoid unnecessary aerosol drug delivery.1,6,7 | Use HFNC for aerosol delivery before the development of severe hypoxemic respiratory failure.6 | Do not use the pMDI to keep the ventilator circuit intact and prevent viral transmission.1,6 | Avoid using pMDI for aerosol drug delivery to prevent viral transmission through cough and airway irritation during device placement directly to the tracheostomy tube.9 |
| Use inhalers for aerosol delivery instead of nebulizers, if the optimum technique can be performed.1,6,7 | Use a mesh nebulizer, place it prior to the humidifier, and keep the reservoir cap closed.1,6,8 | Use a mesh nebulizer, place it prior to the humidifier, and keep the reservoir cap closed after each use.1,6 | Use a mesh nebulizer or a jet nebulizer with a valved T-piece. Attach them to the circuit of the high-flow oxygen delivery device (Figure 2). |
| Attach a filter to the exhalation port of the nebulizer (Figure 3) in patients who are unable to perform the optimum technique with inhalers and when drug formulation is not available as an inhaler.1,5-7 | Make sure HFNC prongs are well-fitted and not loose.1,6,8 | In the absence of a mesh nebulizer, use a jet nebulizer with a valved T-piece during mechanical ventilation.1,6 | Do not use the tracheostomy mask for aerosol therapy.9 Use a T-piece and attach a HEPA filter to the expiratory outlet of the high-flow oxygen delivery system (Figure 2).9 |
| Use a mouthpiece instead of a face mask.5-7 | Place a surgical mask on patient’s face before aerosol therapy.6,8,15 | Attach a HEPA filter to the expiratory limb of the ventilator (Figure 3) and keep the ventilator circuit intact.1,6,17 | Use an unassisted technique to deliver aerosols to the tracheotomized patients instead of the assisted technique unless a filter is attached to the expiratory port of the manual resuscitation bag.9 |
|
For All Patients Receiving Aerosolized Medications |
|||
HFNC = High-Flow Nasal Cannula; pMDI = Pressurized Metered-Dose Inhalers; HEPA = High-Efficiency Particulate Air; PPE = Personal Protective Equipment
Créditos: Comité científico Covid




