En atención a la creciente preocupación sobre la confianza en...
Leer más
Latest Updates on Monoclonal Antibodies
Find the latest COVID-19 news and guidance in Medscape’s Coronavirus Resource Center.
JOHN WHYTE: Welcome, everyone. I’m Dr. John Whyte, Chief Medical Officer at WebMD, and you’re watching Coronavirus in Context, where we try to break down what’s happening with coronavirus and how it impacts your life.
We’ve been talking a lot about the vaccine, as we should, but we can’t forget about treatments. People are still getting COVID. People are still being exposed to COVID. So what are the effective therapies? One of those is monoclonal antibodies. I want to spend some time today talking about how we need to be utilizing them.
So to find out, I’ve gone straight to the source. My guest today is Dr. George Yancopoulos. He’s the president and chief scientific officer of Regeneron. Dr. Yancopoulos, thanks for joining me.
GEORGE YANCOPOULOS: Sure. Glad to be here.
JOHN WHYTE: Let’s start off with reminding everyone, our viewers, some physicians, some patients, some just interested people, what are monoclonal antibodies?
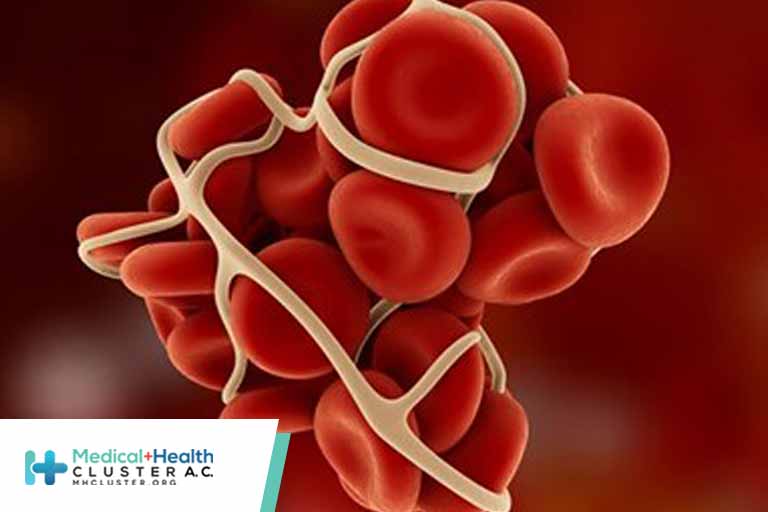
GEORGE YANCOPOULOS: Well, you mentioned vaccines. And obviously, we’re all hoping that vaccines are going to be broadly enough used to generate what’s called herd immunity. What is that? The vaccine makes individuals make their own antibodies against the virus, antibodies that will bind to and kill the virus and provide protection against them.
Now, there are people who will never respond to the vaccine. If you’re immunosuppressed, for example. And those people will not be able to ever generate their own antibodies. In addition, if you haven’t been vaccinated but you’re already sick, you’re already infected, it’s too late for a vaccine because it takes a couple of weeks for the vaccine to induce these protective antibodies.
What we were able to do was essentially clone out the very antibodies, the best of the antibodies that bind and block to the coronavirus, we grow them up in these big bioreactors and then we highly purify them and concentrate them, and we can give it back to individuals as an injection.
So it’s as if they’ve been vaccinated, but immediately acts right away to give them these very antibodies that vaccines induce. So if you’re already infected, it’s too late for the vaccine. But our phase III clinical trials show that it can be very effective to now treat those people and help prevent them from progressing to serious disease. It can also protect people.
JOHN WHYTE: Let’s break all of those down. So there were several emergency use authorizations by the FDA, and sometimes it’s confusing because mono means “one.” When we talk about monoclonal antibodies, we talk about cocktails, which may not be the best term. But let’s kind of go over who currently would benefit most. Let’s start with those persons who are infected who have a positive test. Where do we go from there?
GEORGE YANCOPOULOS: Right. So basically what we know is that if you’re infected and if you’re under one of these high-risk conditions, such as advanced age or a comorbidity such as hypertension, or obesity, or other sort of diseases, you have a significant risk of progressing to hospitalization, severe COVID, and maybe death.
In these people, we actually did a large phase III trial and showed that, in these very people, you’re already infected, it’s too late for the vaccine, what do you do? If you give them our antibody cocktail, these people are protected and have a greater than 70% reduction in their risk of progressing to severe disease requiring hospitalization or death.
So it can really make a difference. I think that the data actually suggests that every infected high-risk person should actually get the cocktail and be treated. It also will decrease the further spread because we’ve also shown that it immediately drops your viral levels and makes you less infectious. And moreover, very importantly, it’s also still active against all of the emerging variants of concern.
JOHN WHYTE: I wanted to ask you about that in terms of the variance, because that’s what everyone is talking about. So tell us again, what do we know about the use of monoclonal antibodies and the variants that we currently know about?
GEORGE YANCOPOULOS: Well, what we know is that, unfortunately, if you just use a single antibody, it’s very likely that that antibody, over time, might lose effectiveness against one or more of these variants. So, in fact, one of the first antibodies that was approved has already been withdrawn because it’s lost its effectiveness against these variants that we’re all hearing about.
However, our people realized early on that these variants were going to occur, and that they prospectively designed a cocktail that is a combination of antibodies, not just one antibody, that would be resistant to variants. They, in fact, predicted the very variants that are emerging today, they predict these almost a year ago now, and showed that if you put the right cocktail together, it could actually protect against these potential variants that would emerge.
And that’s exactly what’s been the case, and so the cocktail is still retaining its effectiveness against, as I said, all the variants of concern that have been identified to date. And so they’re a very, very powerful solution. As I said, if you’re already infected, whether it’s with the variant or whether it’s with the original virus, but increasingly, it’s becoming with the variant, this can decrease your risk of progressing to severe disease, hospitalization, or death.
JOHN WHYTE: Well, let’s talk about the data on prevention, what some scientists will talk to in reference about post-exposure prophylaxis. So those persons who have been exposed, maybe in your household, maybe in an office setting if you return to work, what do we know about that patient population, those people who haven’t tested positive for COVID but have a known exposure to COVID? What’s the role of monoclonal antibodies in that setting?
GEORGE YANCOPOULOS: So there again, so we did one large phase III study in people who are already infected. We also did another one exactly in the setting that you’re describing, the largest phase III study of its kind. And we showed that, for example, if you are living in a household with one infected individual, you have a very high chance of you yourself getting infected.
And as I said, this could be used for just preventing spread among people who are contacts with other people who have had the disease. But increasingly, as hopefully the vaccine is used more and more widely and there is more widespread protection, this can be targeted to individuals who are not mounting their own immune responses, that is, to the vaccine.
And this has been used to great effect using other modalities earlier in terms of ways of protecting immunosuppressed individuals. We now will have a way of potentially giving this very powerful cocktail to immunosuppressed individuals who will never be protected by the vaccine and keep them from getting the infection in the future.
JOHN WHYTE: Now, what about the fact that some people are saying, hey, if I get monoclonal antibodies, then I need to wait 90 days before I can get vaccinated? Do we have any data about that 90 days? Do you expect that to change?
GEORGE YANCOPOULOS: Yeah, it’s a great question. We’re actually doing studies right now to see whether you can be vaccinated more quickly than waiting for that 90 days period. We don’t have data on that right now. So right now, it is a concern that if you get this treatment, you will be protected for a significant amount of time, but it may delay the point at which you can start your vaccination. But we are literally doing studies right now to determine exactly what the minimal interval would have to be that would allow you to then start your vaccination.
JOHN WHYTE: Now, we call it a cocktail. It’s almost as if we’re going to pour it in a glass and drink it. But the delivery mechanism has been somewhat of an obstacle for some folks because typically, requires an infusion center. Not everyone has been able to set that up as quickly as they would have liked. But there is also some data now about, perhaps, being able to do this subcutaneously, under the skin. What do we know about potential changes in the delivery of this therapy?
It appeared that when given that way, the cocktail was very effective, and so we are talking with the FDA about having them authorize subcutaneous administration for both treatment of already infected people as well as for prevention. And we will see what the FDA thinks about that data.
But if, as you said, if the data supports it and the FDA allows it, it will make it a lot easier for this to be used more widely and much more easily both in the treatment setting, you don’t have to go to a hospital, you don’t have to go to an infusion center. There could be a lot of different mechanisms whereby we could understand this could be given. People could get it at home. People could go to a CVS and get an injection.
JOHN WHYTE: And people should know there’s no fee for this, correct?
JOHN WHYTE: But we know they’re still being underutilized. And for our physician viewers, what do they need to know? And then for consumers and patients, what should they be doing in terms of they feel they may be a candidate? How do they find out more?
GEORGE YANCOPOULOS: Yeah. I think that one of the problems has been, obviously, it’s hard to communicate so many messages, and it’s been very important to communicate the need for widespread vaccination, to try to get the numbers down and get the pandemic under control, which appears to be happening.
But we have to recognize there’s still, still 50,000 people getting infected every day. About 30% to 40% of those are high-risk patients and that still results in about 1,000 deaths a day, or 30,000 …
JOHN WHYTE: And 25% of the population says they’re not going to get vaccinated, so we’re still going to have infection.
GEORGE YANCOPOULOS: So we’re going to still have it. So we have to get — we have to do a better job of getting the word out, and that has to be from all sources. It has to happen at the top, from the top government officials, to making people aware that if you are infected or if you didn’t take a vaccine but you are infected now, there is something that could possibly save you, and it’s very effective and it’s very safe. That’s one thing.
And, as you already mentioned, the possibility now that we hope is going to happen in the relatively near term, providing a convenient subcutaneous administration so you don’t have to go to a hospital or an infusion center, is also going to allow much more widespread use.
So I think these are all things that we’re going to have to all do to try to get it used more widely because lives are at stake. There are still tens of thousands of people a month that if we could reduce that by 70%, think about that. That’s saving tens of thousands of lives, and there’s nothing more important than that.
We also have to recognize this is an ongoing problem, as we’re hearing this tragic news from India and so forth, that there’s many places where they’re in a lot worse shape than we’re at. They’re nowhere near vaccinating significant portions of their populations and they’re having tremendous loss of life.
You may have heard that our antibody cocktail was recently authorized by the India Regulatory Authorities, and the U.S. government is actually working with India to figure out how to provide them with some doses of our antibody cocktail to see if we can make a difference there.
So this is going to be an ongoing problem. There is going to be a need for awareness, widespread use within the United States, but also there’s going to be maybe even a bigger need outside of the United States, and as you said, unfortunately, it looks like, for the foreseeable future, we’re going to be dealing with infections.
And whether it’s in the immunocompromised people, remember, there’s 3 to 4 million immunocompromised people in the United States alone. Even if everybody got infected, we would have to do something to protect those people, let alone, unfortunately, if we’re still left with a large segment of the population which ultimately does not get vaccinated.
JOHN WHYTE: Absolutely. The key, as you point out, is to become aware, to get informed. Dr. Yancopoulos, I want to thank you for taking the time today and helping us understand exactly what these therapies are and how we best utilize them.
GEORGE YANCOPOULOS: I appreciate the interest, John. I appreciate helping get the word out because lives are at stake and more broad utilization of this very effective treatment can really make a difference.
JOHN WHYTE: And if you have questions about monoclonal antibodies or other aspects of COVID, drop us a line. You can email me at DrJohn@WebMD.net or post on our social properties, Instagram, Facebook, and Twitter. Thanks for watching.
https://www.medscape.com/viewarticle/950687?src=soc_fb_210509_mscpedt_news_mdscp_whyte&faf=1#vp_1
Créditos: Comité científico Covid




